Arteriovenous malformations (AVMs) are complex and often misunderstood medical conditions that can manifest with a broad spectrum of symptoms. For those affected by AVMs and their loved ones, understanding the diverse presentation of symptoms is crucial for prompt diagnosis and effective management. This expansive guide serves to communicate the various signs and indicators of AVMs, catering to the interests of health enthusiasts, patients, and medical professionals in the field.
Introduction to AVM and Early Symptoms
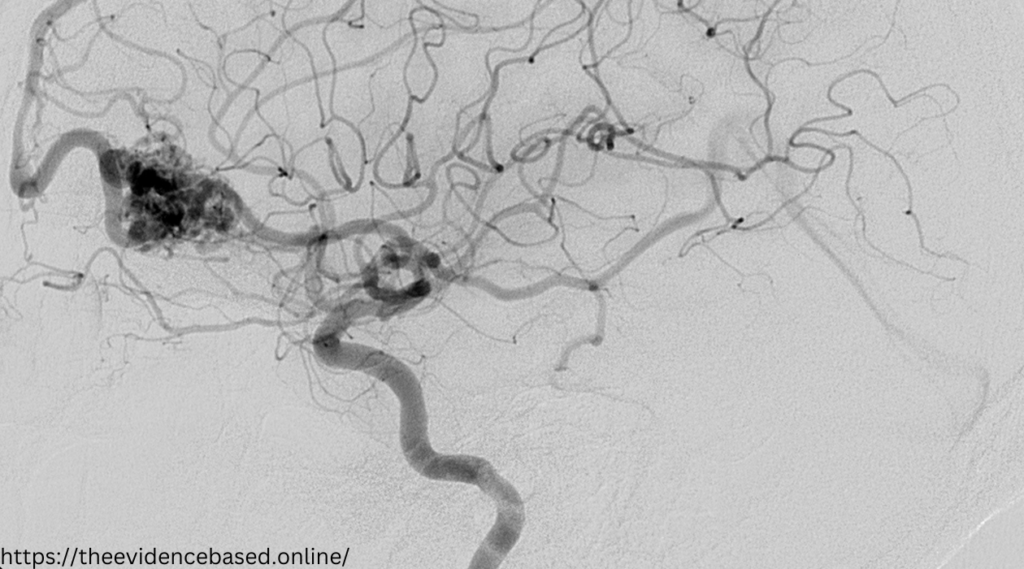
Arteriovenous Malformations (AVMs) are abnormal connections between arteries and veins, which usually develop before birth and can occur in any part of the body. In the context of neurological AVMs, these irregularities predominantly reside within the brain or spinal cord, affecting blood flow and potentially leading to serious health implications.
Identifying AVM symptoms early is pivotal in ensuring that appropriate medical actions are taken promptly. While the symptoms can vary from person to person, recognizing the early signs can significantly impact one’s quality of life and treatment outcomes.
Common Symptoms of AVM
Many AVM patients experience chronic or rapidly escalating symptoms that can have a profound impact on daily life. One of the most universally reported symptoms is persistent headaches, not unlike migraines, often worsened by physical activity, coughing, or sudden movement.
Seizures are another classic symptom, affecting a significant portion of AVM patients. These can manifest as episodic loss of awareness, convulsions, or sensory distortions. Neurological deficits, characterized by muscle weakness, numbness or tingling, and difficulty with speech or movement, also frequently occur.
Cognitive changes, such as memory loss, difficulties with attention, and changes in the thought process, are some of the least specific yet highly debilitating symptoms.
Lesser-Known Symptoms and Signs
In addition to the typical manifestations of AVMs, several lesser-known symptoms may indicate an AVM is present. Dizziness, vertigo, and balance disturbances can occur. Vision problems are also reported, ranging from blurred vision to visual field defects.
Speech difficulties can range from the inability to produce speech to a slurred or slow verbal output. Accompanying this, behavioral changes, such as aggression, apathy, or mood swings, are documented in a subset of AVM patients.
Diagnosis and Treatment Options
Diagnosis often begins with a clinical evaluation, followed by various imaging tests such as CT scans and MRI to confirm the presence and location of the AVM. Upon confirmation, a multidisciplinary team of physicians comprising neurologists, neurosurgeons, interventional radiologists, and other specialists will work with the patient to determine the most suitable treatment course.
Surgical options, including resection and AVM removal, may be recommended. Embolization, where a material is used to block the blood vessels supplying the AVM, is a non-invasive procedure often utilized. Alternatively, radiation therapy can be considered to shrink the AVM over time.
Living with AVM
Adjusting to life with an AVM involves both medical management and lifestyle changes. It’s often encouraged for patients to join support groups, access resources, and consider therapy to cope with the implications of the diagnosis.
Lifestyle modifications, including stress management techniques, regular exercise, and maintaining a healthy diet, are also essential for long-term well-being. Monitoring and follow-up care are routine aspects of living with AVM since periodic imaging and clinical evaluations are crucial for detecting any changes in the AVM’s condition.
Conclusion
Understanding the symptoms of AVM is a complex yet empowering endeavor. It allows for a proactive approach to healthcare and provides a foundation for informed discussions with healthcare professionals. By staying knowledgeable about the signs and symptoms, individuals and their support networks can act swiftly and decisively, offering the best chance at managing and treating AVMs effectively.